_MECHANISMS OF ACTION OF ANTIMICROBIAL DRUGS
Selective Toxicity. Selective toxicity
is the property of an ideal antimicrobial
agent. Selective toxicity means that the drug is harmful to a parasite but not to the host. Usually the effect is relative rather absolute, i.e. a drug in a
concentration tolerated by the host may damage an infecting microorganism.
Selective toxicity may be a function
of a specific receptor required for drug
attachment, or it may depend on inhibition of biochemical events essential to the organism but not to the
host. The mechanisms are discussed
under four headings: (1) Inhibition of cell wall synthesis, (2) Inhibition of cell membrane function, (3) Inhibition of protein synthesis, and
(4) Inhibition of nucleic acid synthesis.
Classification on mode of Action:
1. Inhibition of cell wall synthesis. Penicillins, cephalosporin, vancomycin, bacitracin, cycloserin are examples.
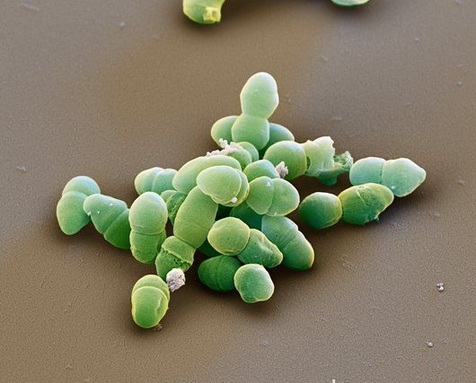
All (3-Iactarn drugs like penicillins, cephalosporins are selective inhibitors of bacterial cell wall synthesis and therefore active against growing bacteria. Mechanism of action: Initial step is the binding of the drug to specific drug receptor PBPs (Penicillin- binding proteins) on bacteria. There are 3 to 6 PBPs having different effects. At least some of which are enzymes involved in transpeptidation (cross-linking) reactions. After attachment, peptidoglycan synthesis is inhibited as final transpeptidation is blocked. Then there occurs inactivation of an inhibitor of autolytic enzyme in the cell wall. This activates the autolytic enzymes in the cell wall that results in lysis resulting in bacterial death. Organisms with defective autolysin function are inhibited but not killed by l3dactam drugs, and they are said to be "tolerant".
The Gram-positive and Gram-negative bacteria differ in susceptibility to penicillins or cephalosporins on structural differences in their cell walls that decide binding, penetration, and activity of the drugs. The differences in cell wall are in the amount of peptidoglycan, presence of receptors and lipids, nature of cross-linking and activity of autolytic enzymes. Peptidoglycan layer of the cell wall is much thicker in Gram-positive than in Gram-negative bacteria.
Lack of toxicity of p-lactam drugs to animal cells is attributed to the absence of bacterial type cell wall with its peptidoglycan in animal cells.
Extended-spectrum P lactum (ESBLs) are enzymes that mediate resistance to extended-spectrum (third generation) cephalosporins (e.g., ceftazidime, cefotaxime, and ceftriaxone) and monobactams (e.g., aztreonam) but do not affect cephamycins (e.g., cefoxitin and cefotetan) or carbapenems (e.g., meropenem or imipenem). Production of ESBLs can be screened by broth microdilution and disk diffusion screening tests using selected antimicrobial agents.
Classification on mode of Action:
1. Inhibition of cell wall synthesis. Penicillins, cephalosporin, vancomycin, bacitracin, cycloserin are examples.
All (3-Iactarn drugs like penicillins, cephalosporins are selective inhibitors of bacterial cell wall synthesis and therefore active against growing bacteria. Mechanism of action: Initial step is the binding of the drug to specific drug receptor PBPs (Penicillin- binding proteins) on bacteria. There are 3 to 6 PBPs having different effects. At least some of which are enzymes involved in transpeptidation (cross-linking) reactions. After attachment, peptidoglycan synthesis is inhibited as final transpeptidation is blocked. Then there occurs inactivation of an inhibitor of autolytic enzyme in the cell wall. This activates the autolytic enzymes in the cell wall that results in lysis resulting in bacterial death. Organisms with defective autolysin function are inhibited but not killed by l3dactam drugs, and they are said to be "tolerant".
The Gram-positive and Gram-negative bacteria differ in susceptibility to penicillins or cephalosporins on structural differences in their cell walls that decide binding, penetration, and activity of the drugs. The differences in cell wall are in the amount of peptidoglycan, presence of receptors and lipids, nature of cross-linking and activity of autolytic enzymes. Peptidoglycan layer of the cell wall is much thicker in Gram-positive than in Gram-negative bacteria.
Lack of toxicity of p-lactam drugs to animal cells is attributed to the absence of bacterial type cell wall with its peptidoglycan in animal cells.
Extended-spectrum P lactum (ESBLs) are enzymes that mediate resistance to extended-spectrum (third generation) cephalosporins (e.g., ceftazidime, cefotaxime, and ceftriaxone) and monobactams (e.g., aztreonam) but do not affect cephamycins (e.g., cefoxitin and cefotetan) or carbapenems (e.g., meropenem or imipenem). Production of ESBLs can be screened by broth microdilution and disk diffusion screening tests using selected antimicrobial agents.
_ 2. Alteration of cell membrane
function. Polymyxin, amphotericin B, imidazole are examples.
These drugs act by disruption of the functional integrity of the cytoplasmic membrane. Macromolecules and ions escape from the cell causing cell damage or death. Selective chemotherapy is possible as the cytoplasmic membrane of bacteria and fungi has a structure different from that of animal cells, and can be more readily disrupted by certain chernothe rape utics.
3. Inhibition of protein synthesis. These drugs inhibit protein synthesis in bacteria. Bacteria have 70S ribosomes, whereas mammalian cells have 80S ribosomes. Subunits of each type of ribosome, their chemical composition, and functional specifities differ. Thus a drug can inhibit protein synthesis in bacterial ribosomes but not in mammalian ribosomes.
(a) Action on 50S ribosomal subunit. Chloramphenicol, erythromycin and chindamycin are examples.
(b) Action on 30S ribosomal subunit. Tetracycline and aminoglycosides are examples.
4. Inhibition of nucleic acid synthesis. These drugs inhibit nucleic acid synthesis by different mechanisms. (a) Inhibition of nucleotide synthesis. Sulphonamides, trimethoprin Sulphonamides compete for the enzyme required for essential metabolite PABA involved in the synthesis of folic acid needed for synthesis of nucleic acid. (b) Inhibition of DNA synthesis. Quinolones block DNA gyrase. (c) Inhibition of mRNA synthesis- Rifampin.
These drugs act by disruption of the functional integrity of the cytoplasmic membrane. Macromolecules and ions escape from the cell causing cell damage or death. Selective chemotherapy is possible as the cytoplasmic membrane of bacteria and fungi has a structure different from that of animal cells, and can be more readily disrupted by certain chernothe rape utics.
3. Inhibition of protein synthesis. These drugs inhibit protein synthesis in bacteria. Bacteria have 70S ribosomes, whereas mammalian cells have 80S ribosomes. Subunits of each type of ribosome, their chemical composition, and functional specifities differ. Thus a drug can inhibit protein synthesis in bacterial ribosomes but not in mammalian ribosomes.
(a) Action on 50S ribosomal subunit. Chloramphenicol, erythromycin and chindamycin are examples.
(b) Action on 30S ribosomal subunit. Tetracycline and aminoglycosides are examples.
4. Inhibition of nucleic acid synthesis. These drugs inhibit nucleic acid synthesis by different mechanisms. (a) Inhibition of nucleotide synthesis. Sulphonamides, trimethoprin Sulphonamides compete for the enzyme required for essential metabolite PABA involved in the synthesis of folic acid needed for synthesis of nucleic acid. (b) Inhibition of DNA synthesis. Quinolones block DNA gyrase. (c) Inhibition of mRNA synthesis- Rifampin.