_RESISTANCE TO ANTIMICROBIAL DRUGS
_ A. Mechanisms of
Drug Resistance. Microoganisms exhibit
resistance to antimicrobial drugs by different mechanisms.
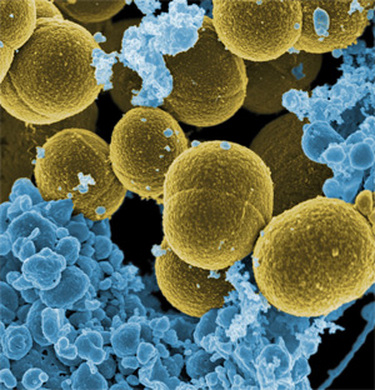
1. Microorganisms produce enzymes that destroy the active drug. Examples: P-lactamases (Penicillinases) produced by certain bacteria destroy penicillin. Staphylococci resistant to penicillin G produce a P-lactamase that destroys the drug. Other P-lactamases are produced by Gram-negative rods.
2. Microorganisms change their permeability to the drug, e.g. tetracycline accumulate in susceptible bacteria but not in resistant bacteria.
3. Microorganisms develop an altered metabolic pathway that bypasses the reaction inhibited by the drug. Sulphonamide resistant bacteria do not require extracellular PABA, but can utilize preformed folic acid.
4. Microorganisms develop an altered structural target for the drug: Erythromycin resistant organisms have on altered receptor on the 50S subunit of the ribosome. Aminoglycosidesresistant is due to alteration or loss of a specific protein in the 30S subunit of the bacterial ribosome that serve as a binding site in susceptible organisms. Resistance to some penicillins and cephalosporins occurs due to alteration or loss of PBPs.
5. Microorganisms develop an altered enzyme that can perform its metabolic function but is much less affected by the drug.
1. Microorganisms produce enzymes that destroy the active drug. Examples: P-lactamases (Penicillinases) produced by certain bacteria destroy penicillin. Staphylococci resistant to penicillin G produce a P-lactamase that destroys the drug. Other P-lactamases are produced by Gram-negative rods.
2. Microorganisms change their permeability to the drug, e.g. tetracycline accumulate in susceptible bacteria but not in resistant bacteria.
3. Microorganisms develop an altered metabolic pathway that bypasses the reaction inhibited by the drug. Sulphonamide resistant bacteria do not require extracellular PABA, but can utilize preformed folic acid.
4. Microorganisms develop an altered structural target for the drug: Erythromycin resistant organisms have on altered receptor on the 50S subunit of the ribosome. Aminoglycosidesresistant is due to alteration or loss of a specific protein in the 30S subunit of the bacterial ribosome that serve as a binding site in susceptible organisms. Resistance to some penicillins and cephalosporins occurs due to alteration or loss of PBPs.
5. Microorganisms develop an altered enzyme that can perform its metabolic function but is much less affected by the drug.
_ B. Origin of Drug
Resistance. The origin of drug resistance may be genetic or
nongenetic.
1. Genetic Origin of Drug Resistance. Most drug-resistant microorganisms emerge as a result of genetic change and subsequent selection processes by antimicrobial drugs. Genetic mechanism may be chromosomal or extra-chromosomal.
(i) Chromosomal Resistance. Chromosome-mediated resistance occurs by spontaneous mutation in a locus that controls susceptibility to the drug. The antimicrobial drug serves as a selecting mechanism to suppress susceptible organisms and favor the growth of drug-resistant mutants. Spontaneous mutation is not a frequent cause of the clinical drug resistance in a given patient. But it occurs with high frequency to rifampicin. Mutation can result in the loss of PBPs, making such mutants resistant to a-Iactam drugs. ExamplesRifampicin, streptomycin, erythromycin. Resistance of M. tuberculosis to rifampicin is caused by mutation in RNA polymerase and that to isoniazid by mutation in catalase.
(ii)Extrachromosomal Resistance
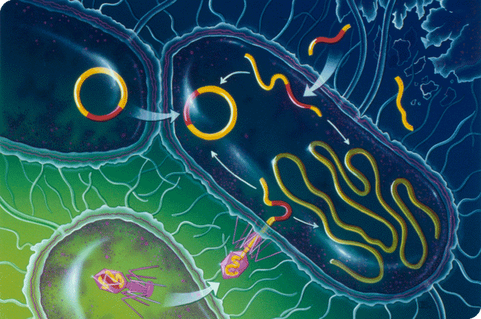
(a) Plasmid Resistance. This occurs by the extrachromosomal genetic elements called plasmid. Plasmidmediated drug resistance is more common than that of chromosome. R factors (drug resistance plasmids) are a class of plasmids that carry genes for resistance to antimicrobial drugs. A single plasmid can carry genes that code for resistance to several drugs (multi-drug resistance -MDR) such as streptomycin, chloramphenicol, tetracycline and sulphonamides. Plasmid genes control the formation of enzymes capable of destroying the antimicrobial drugs, e.g. Plactamases destroy P-lactam ring of penicillins and cephalosporins.
(b) Transposon Resistance.
Genetic material responsible for antimicrobial resistance of a donor cell may be transferred to a sensitive recipient cell, and the recipient cell thus becomes resistant to the drug(s). The intercellular transfer of genetic material may occur by : (a) Conjugation, Conjugation is the most important of these mechanisms for the transfer of antimicrobial resistance. In most cases of conjugation the transferable DNA is plasmid, but chromosomal DNA may also be transferred, (b) Transduction. Transduction is the transfer of cell DNA by means of a bacterial virus (bacteriophage, phage). Transfer of gene for Beta lactamase production is mediated by bacteriophage, and (c) Transformation. It is a natural occurrence, and is a direct uptake of donor DNA by recipient cells.
1. Genetic Origin of Drug Resistance. Most drug-resistant microorganisms emerge as a result of genetic change and subsequent selection processes by antimicrobial drugs. Genetic mechanism may be chromosomal or extra-chromosomal.
(i) Chromosomal Resistance. Chromosome-mediated resistance occurs by spontaneous mutation in a locus that controls susceptibility to the drug. The antimicrobial drug serves as a selecting mechanism to suppress susceptible organisms and favor the growth of drug-resistant mutants. Spontaneous mutation is not a frequent cause of the clinical drug resistance in a given patient. But it occurs with high frequency to rifampicin. Mutation can result in the loss of PBPs, making such mutants resistant to a-Iactam drugs. ExamplesRifampicin, streptomycin, erythromycin. Resistance of M. tuberculosis to rifampicin is caused by mutation in RNA polymerase and that to isoniazid by mutation in catalase.
(ii)Extrachromosomal Resistance
(a) Plasmid Resistance. This occurs by the extrachromosomal genetic elements called plasmid. Plasmidmediated drug resistance is more common than that of chromosome. R factors (drug resistance plasmids) are a class of plasmids that carry genes for resistance to antimicrobial drugs. A single plasmid can carry genes that code for resistance to several drugs (multi-drug resistance -MDR) such as streptomycin, chloramphenicol, tetracycline and sulphonamides. Plasmid genes control the formation of enzymes capable of destroying the antimicrobial drugs, e.g. Plactamases destroy P-lactam ring of penicillins and cephalosporins.
(b) Transposon Resistance.
Genetic material responsible for antimicrobial resistance of a donor cell may be transferred to a sensitive recipient cell, and the recipient cell thus becomes resistant to the drug(s). The intercellular transfer of genetic material may occur by : (a) Conjugation, Conjugation is the most important of these mechanisms for the transfer of antimicrobial resistance. In most cases of conjugation the transferable DNA is plasmid, but chromosomal DNA may also be transferred, (b) Transduction. Transduction is the transfer of cell DNA by means of a bacterial virus (bacteriophage, phage). Transfer of gene for Beta lactamase production is mediated by bacteriophage, and (c) Transformation. It is a natural occurrence, and is a direct uptake of donor DNA by recipient cells.
_ 2. Nongenetic Origin of Drug
Resistance. This may be due to:
(i) Metabolic inactivity. Most antibacterial drugs act when the microorganisms multiply actively. As such they become resistant to the drug when metabolically inactive, i.e. not multiplying. However, their offsprings are fully susceptible. Example: "Persisting" organisms like mycobacteria survive in tissues for many years after infection and do not multiply. They can not be eradicated by drugs. But if they start to multiply then they become fully susceptible to the same drugs.
(ii) Loss of specific target structure. Microorganisms become resistant due to loss of a specific target structure. Example: During penicillin administration, penicillin-susceptible organisms may change to cell wall deficient L forms, and become resistant to cell wall-inhibitor drugs (penicillins, cephalosporins).
(iii)Infection at sites where antimicrobials are excluded or are not active.
NOTE: Examples:
A. Resistance to penicillins can be due to:
1. Production of P-lactamases by staphylococci, gonococci, Gram-negative rods, and others. About 50 fl-lactamases are known and under the control of plasmids.
2. Altered or lack of PBPs. Mostly under the control of chromosomes.
3. Failure of activation of autolytic enzymes in cell wall.
4. Failure to synthesize peptidoglycans, e.g. in L forms, mycoplasma.
B. Resistance to cephalosporins can be due to
1. Poor permeation of bacteria by the drug
2. Lack of PBP
3. Degradation of drug by β-lactamases.
(i) Metabolic inactivity. Most antibacterial drugs act when the microorganisms multiply actively. As such they become resistant to the drug when metabolically inactive, i.e. not multiplying. However, their offsprings are fully susceptible. Example: "Persisting" organisms like mycobacteria survive in tissues for many years after infection and do not multiply. They can not be eradicated by drugs. But if they start to multiply then they become fully susceptible to the same drugs.
(ii) Loss of specific target structure. Microorganisms become resistant due to loss of a specific target structure. Example: During penicillin administration, penicillin-susceptible organisms may change to cell wall deficient L forms, and become resistant to cell wall-inhibitor drugs (penicillins, cephalosporins).
(iii)Infection at sites where antimicrobials are excluded or are not active.
NOTE: Examples:
A. Resistance to penicillins can be due to:
1. Production of P-lactamases by staphylococci, gonococci, Gram-negative rods, and others. About 50 fl-lactamases are known and under the control of plasmids.
2. Altered or lack of PBPs. Mostly under the control of chromosomes.
3. Failure of activation of autolytic enzymes in cell wall.
4. Failure to synthesize peptidoglycans, e.g. in L forms, mycoplasma.
B. Resistance to cephalosporins can be due to
1. Poor permeation of bacteria by the drug
2. Lack of PBP
3. Degradation of drug by β-lactamases.